What Works? Strategies to Improve Rural Health
This report outlines key steps toward building healthy communities along with some specific policies and programs that can improve health in rural areas.
Creating Healthier Rural Communities
The County Health Rankings & Roadmaps program helps communities identify and implement solutions that make it easier for people to be healthy in their neighborhoods, schools, and workplaces. Ranking the health of nearly every county in the nation, the County Health Rankings illustrate what we know when it comes to what is keeping people healthy or making people sick. The Roadmaps show what we can do to create healthier places to live, learn, work, and play. The Robert Wood Johnson Foundation collaborates with the University of Wisconsin Population Health Institute to bring this program to communities across the nation.
Each year, the County Health Rankings bring actionable data to counties across the country, serving as a call to action to improve local health. The 2016 Rankings include an in-depth examination of the differences in health between rural and urban counties, with some revealing findings:
- Rural counties have had the highest rates of premature death for many years, lagging far behind other counties.
- While urban counties continue to show improvement, overall rates of premature death are worsening in rural counties.
- Nearly one in five rural counties has experienced worsening premature death rates over the past decade.
There is no single factor that explains the significant differences in health between rural and other types of counties. So where do you start? And how do you know what is going to make a difference for your community?
This report outlines key steps toward building healthy communities—rural, urban, and anywhere in between—along with some specific policies and programs that can improve health. Policies and programs that have been tested in rural communities are highlighted throughout the report.
You can find more information about policies and programs that can improve health on our website.
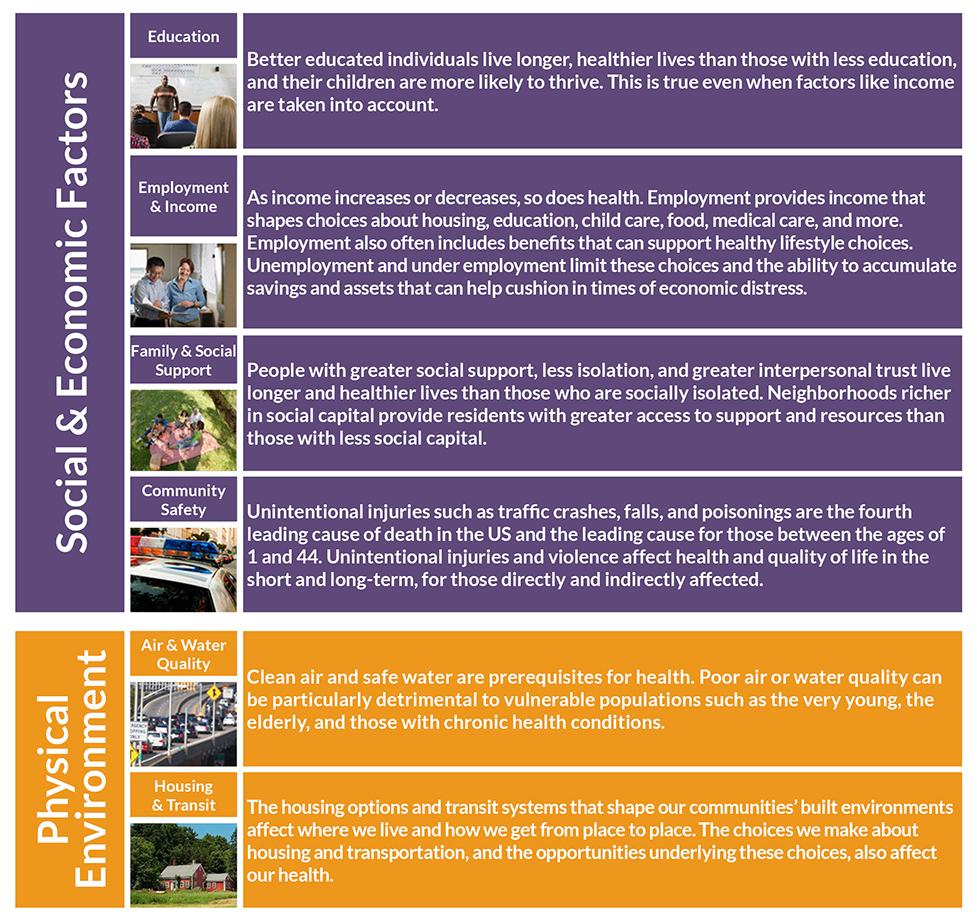
What Influences Health?
Health is about more than what happens at the doctor’s office. The places where we live, learn, work, and play, the choices we make, and the opportunities we have all matter to our physical, mental, and social well-being.
Getting Started
Finding policies and programs that will work for your community requires a firm understanding of local priorities, needs, assets, and values. To get started:
- Think broadly about the factors that influence health. Considering the upstream factors that lead to longer, healthier lives can help identify root causes of your community’s challenges. These upstream drivers include education and income and the many other factors described in this report.
- Assess needs and resources. Take stock of your community’s needs, resources, strengths, assets, and values. Understand what helps and what can deter progress toward improving health in your community.
- Focus on what’s most important. Once you’ve accounted for your community’s needs and resources, it’s time to decide which problem(s) to tackle. Without focus, all issues seem equally important. Taking time to set priorities will ensure that you direct your valuable and limited resources to the most important issues.
- Choose the right policies and programs for your community. Taking time to choose policies and programs that have been shown to work in real life and that are a good fit for your community’s priorities and culture will maximize your chances of success. Focusing on policy, systems, and environmental changes—or implementing programs in a systematic way—can lead to the most substantial improvements over time.
Each step of the way, you’ll want to:
- Engage a variety of stakeholders. Harnessing the collective power of local leaders, partners, and community members, including those who experience the worst conditions for good health, is key to making change.
- Communicate. Consider how you will get your most important messages to the people who matter. Have plans to communicate with others in your community, and with your partners, and put those plans in action.
Efforts to ensure that everyone—especially those disproportionately affected by poor health outcomes—has a say in your community health improvement work can help to close gaps in health outcomes and improve health for all.
Visit the Roadmaps to Health Action Center for more guidance about implementing your selected strategies and evaluating your successes.
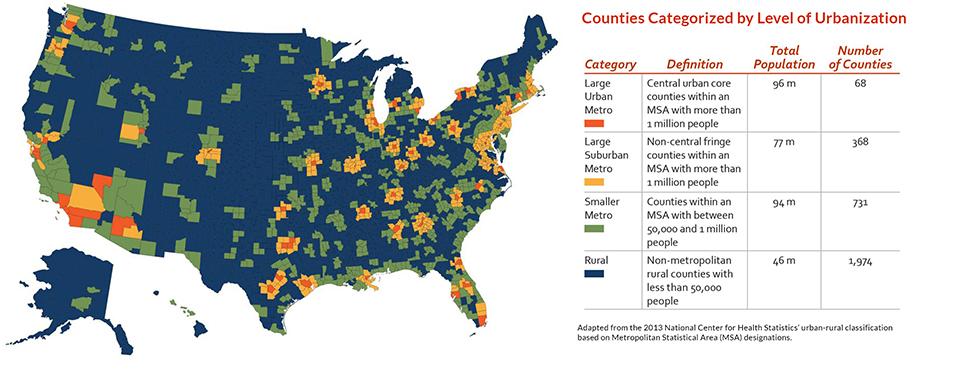
Rural Places
There are various ways to define “rural.” The figures presented in this report use a classification adapted from the National Center for Health Statistics’ rural-urban classification based on Metropolitan Statistical Area (MSA) designations. Although counties are classified into one category on the map above and table to the right, many counties include areas that are urban and areas that are rural (e.g., counties classified as Large Urban Metro often include a mix of areas that are urban and rural). Thinking carefully about the ranges of population density in your community can help you best use the steps and strategies in this report to improve health locally.
Finding a Strategy that Works
Once you know your goal, it’s time to choose a policy or program that will help you achieve it. A good first step is to explore strategies that have worked in other communities or are recommended by unbiased experts. With evidence ratings, literature summaries, and implementation resources for over 360 strategies (i.e., policies, programs, systems and environmental changes), What Works for Health (WWFH) is a great place to start. WWFH is available on our website.
In WWFH, you will find in-depth information for a variety of policies and programs that can improve the many factors that influence health, including health behaviors, clinical care, the physical environment, and social and economic circumstances. For each policy and program you will find:
- Beneficial outcomes (i.e., the benefits the strategy has been shown to achieve as well as other outcomes it may affect)
- Key points from relevant literature (e.g., populations affected, key components of successful implementation, cost-related information, etc.)
- Implementation examples and resources, toolkits, and other information to help you get started
- An indication of the strategy’s likely impact on the gaps or disparities in outcomes that are experienced by
- different groups of people (e.g., members of different racial and ethnic or socio-economic groups)
You can use WWFH to find ideas to support important initiatives in your community, such as:
- Preparing and strengthening the local workforce
- Reducing injuries
- Improving access to high quality health care
- Improving diet and increasing exercise
The following sections outline examples of policies and programs that communities around the country are using to support each of these goals. Many of these strategies have been tested or implemented in rural areas.
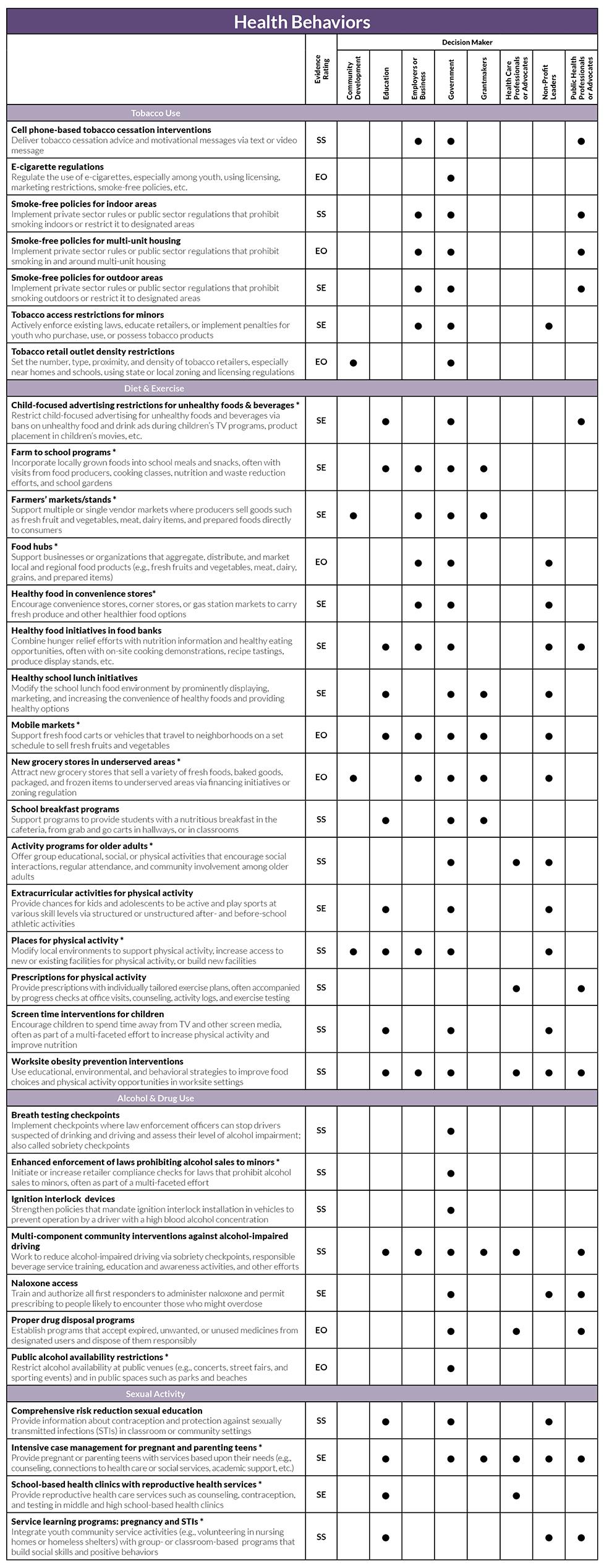
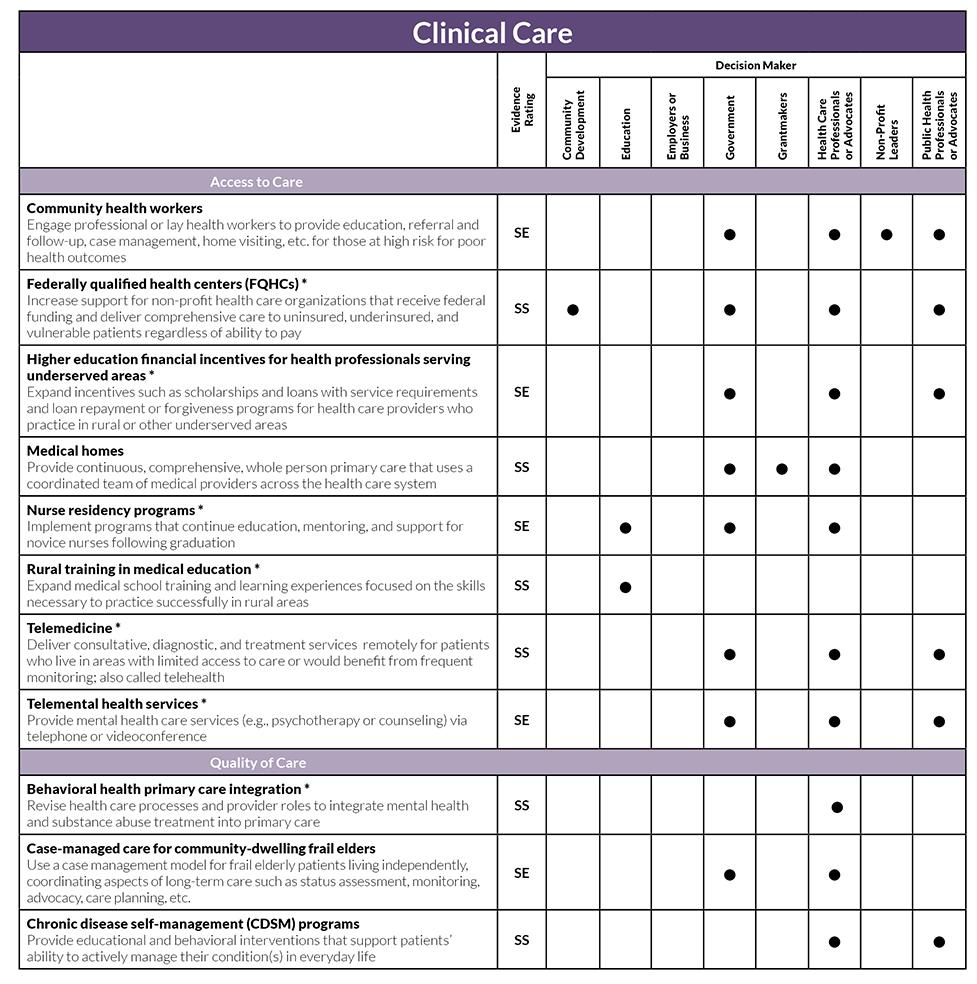
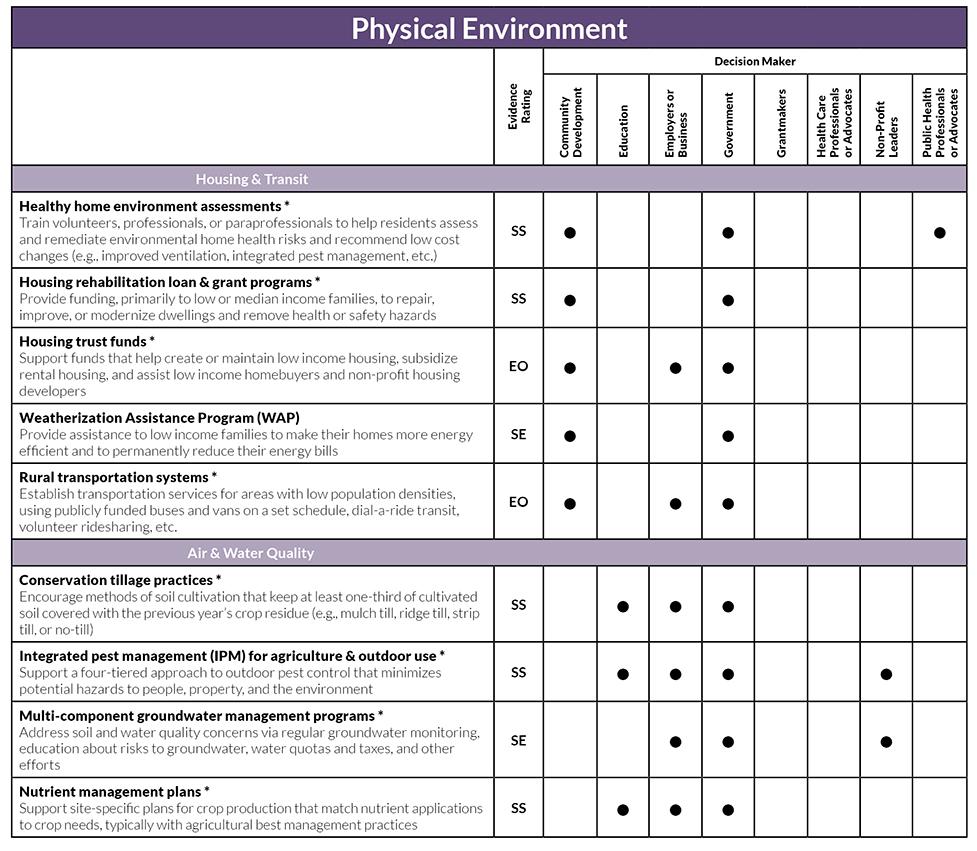
Evidence Rating
WWFH includes six evidence of effectiveness ratings. Each strategy is rated based on the quantity, quality, and findings of relevant research.
Ratings include:
- Scientifically Supported (SS): Strategies with this rating are most likely to make a difference. These strategies have been tested in multiple robust studies with consistently positive results.
- Some Evidence (SE): Strategies with this rating are likely to work, but further research is needed to confirm effects. These strategies have been tested more than once and results trend positive overall.
- Expert Opinion (EO): Strategies with this rating are recommended by credible, impartial experts but have limited research documenting effects; further research, often with stronger designs, is needed to confirm effects.
- Insufficient Evidence (IE): Strategies with this rating have limited research documenting effects. These strategies need further research, often with stronger designs, to confirm effects.
- Mixed Evidence (Mixed): Strategies with this rating have been tested more than once and results are inconsistent; further research is needed to confirm effects.
- Evidence of Ineffectiveness (EI): Strategies with this rating are not good investments. These strategies have been tested in multiple studies with consistently negative or harmful results.
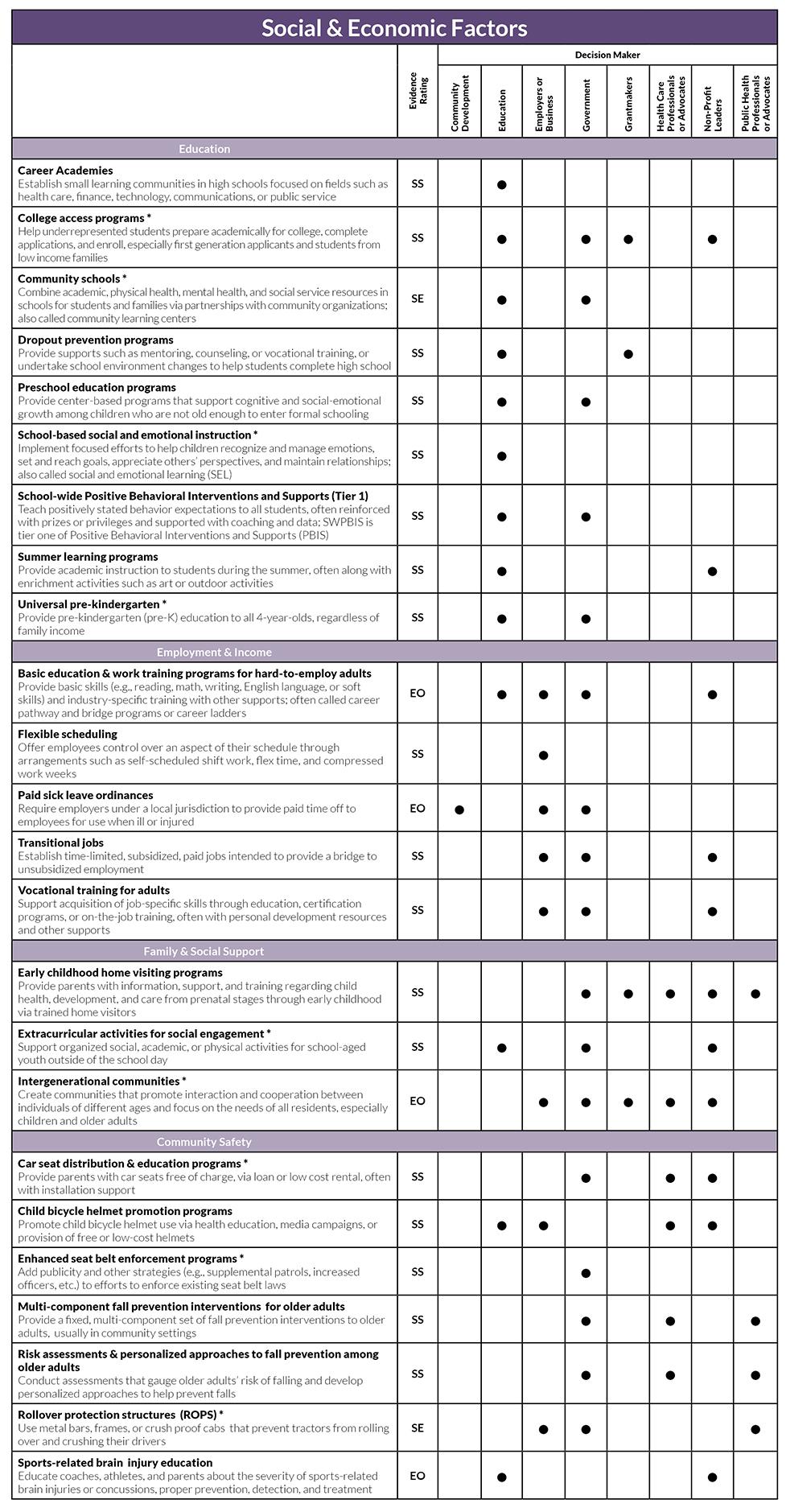
What’s Working to Prepare and Strengthen Local Workforces?
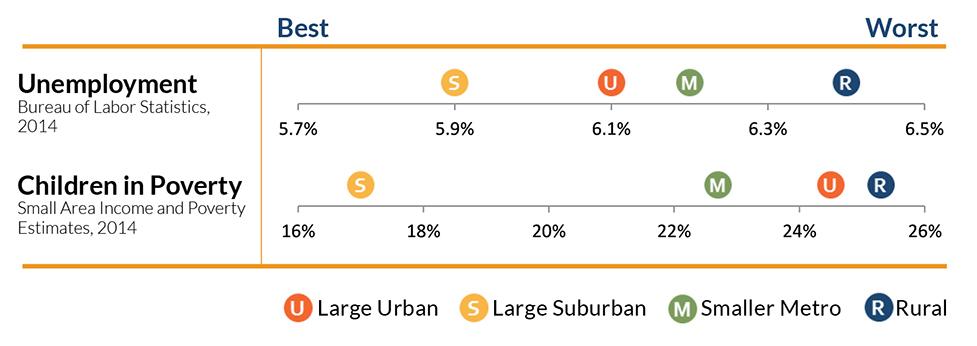
A strong local economy supports employment opportunities and healthy lifestyle choices for individuals and families, and is linked to lower rates of poverty and unemployment. Poverty and unemployment rates are higher in rural areas than in urban and suburban areas. Employers, educational institutions, and community members can work together to increase job skills for residents, enhance local employment opportunities, and set children on a path towards academic and financial success. Examples include:
Career Academies (SS)
Establish small learning communities in high schools focused on fields such as health care, finance, technology, communications, or public service
College access programs (SS) *
Help underrepresented students prepare academically for college, complete applications, and enroll, especially first generation applicants and students from low income families
Dropout prevention programs (SS)
Provide supports such as mentoring, counseling, or vocational training, or undertake school environment changes to help students complete high school
Flexible scheduling (SS)
Offer employees control over an aspect of their schedule through arrangements such as self-scheduled shift work, flex time, and compressed work weeks
Preschool education programs (SS)
Provide center-based programs that support cognitive and social-emotional growth among children who are not old enough to enter formal schooling
Rural transportation systems (EO) *
Establish transportation services for areas with low population densities, using publicly funded buses and vans on a set schedule, dial-a-ride transit, volunteer ridesharing, etc.
School-based social and emotional instruction (SS) *
Implement focused efforts to help children recognize and manage emotions, set and reach goals, appreciate others’ perspectives, and maintain relationships; also called social and emotional learning (SEL)
Transitional jobs (SS)
Establish time-limited, subsidized, paid job opportunities to provide a bridge to unsubsidized employment
* What Works for Health materials include rural-focused resources or studies
What’s Working to Reduce Injuries?
Unintentional injuries such as traffic crashes, falls, and poisonings are the fourth leading cause of death in the US and the leading cause for those between the ages of 1 and 44. Injury death rates are highest in rural areas, largely due to traffic accidents, drug overdoses, and other unintentional injuries. Communities can help protect their residents by adopting and implementing policies and programs to prevent unintentional injuries and violence of all types. Examples include:
Breath testing checkpoints (SS)
Implement checkpoints where law enforcement officers can stop drivers suspected of drinking and driving and assess their level of alcohol impairment; also called sobriety checkpoints
Enhanced seat belt enforcement programs (SS) *
Add publicity and other strategies (e.g., supplemental patrols, increased officers, etc.) to efforts to enforce existing seat belt laws
Multi-component fall prevention interventions for older adults (SS)
Provide a fixed, multi-component set of fall prevention interventions to older adults, usually in community settings
Naloxone access (SE)
Train and authorize all first responders to administer naloxone and permit prescribing to people likely to encounter those who might overdose
Risk assessments & personalized approaches to fall prevention among older adults (SS)
Conduct assessments that gauge older adults’ risk of falling and develop personalized approaches to help prevent falls
Speed enforcement detection devices (SE)
Use devices such as speed cameras, radar, etc. to enforce speed limits; devices can be permanent fixtures or be used manually by law enforcement officers
* What Works for Health materials include rural-focused resources or studies
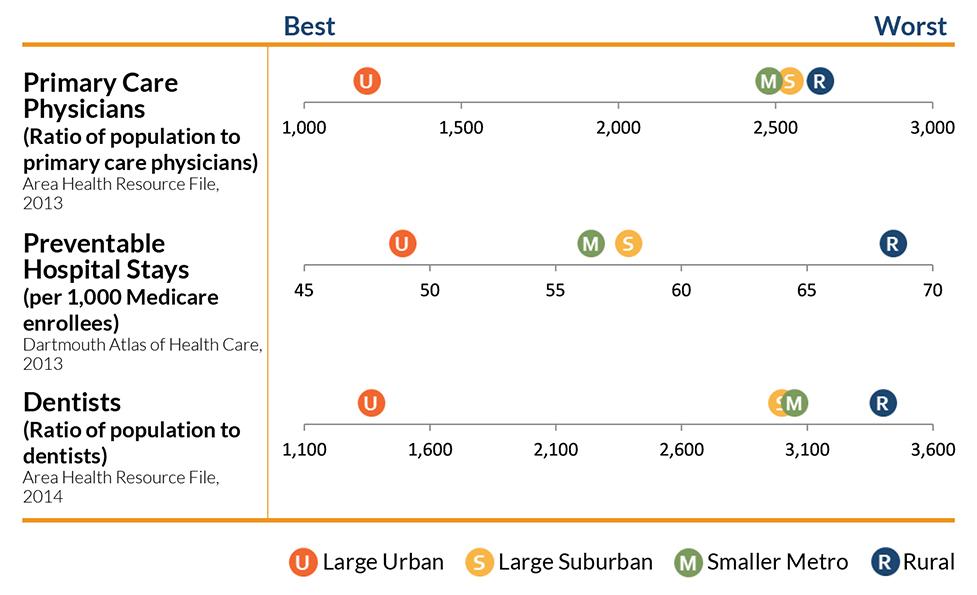
What’s Working to Improve Access to High Quality Health Care?
Access to affordable, quality health care is important to physical, social, and mental health. High quality care in outpatient and inpatient settings can help protect and improve health and reduce the likelihood of receiving
unnecessary or inappropriate care. However, such care can be harder to attain in rural areas than in urban or suburban areas. Adopting and implementing strategies that reduce barriers to care and better match providers to community needs can increase access to high quality care. Examples include:
Community health workers (SE)
Engage professional or lay health workers to provide education, referral and follow-up, case management, home visiting, etc. for those at high risk for poor health outcomes
Federally qualified health centers (SS) *
Increase support for non-profit health care organizations that receive federal funding and deliver comprehensive care to uninsured, underinsured, and vulnerable patients regardless of ability to pay
Higher education financial incentives for health professionals serving underserved areas (SE) *
Expand incentives such as scholarships and loans with service requirements and loan repayment or forgiveness programs for health care providers who practice in rural or other underserved areas
Rural training in medical education (SS) *
Expand medical school training and learning experiences focused on the skills necessary to practice successfully in rural areas
School dental programs (SS) *
Provide sealants, fluoride treatment, screening, and other basic dental care on school grounds via partnerships with dental professionals
Telemedicine (SS) *
Deliver consultative, diagnostic, and treatment services remotely for patients who live in areas with limited access to care or would benefit from frequent monitoring; also called telehealth
Telemental health services (SE) *
Provide mental health care services (e.g., psychotherapy or counseling) via telephone or videoconference
* What Works for Health materials include rural-focused resources or studies
What’s Working to Improve Diet and Exercise?
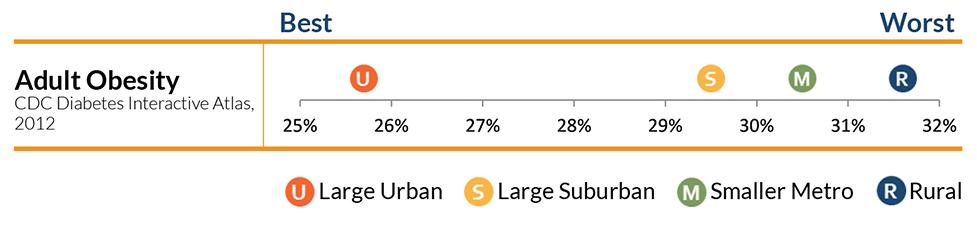
Good nutrition is essential for health, growth, and development. Excessive calorie consumption, however, can lead to overweight and obesity and associated health risks, especially when paired with too little physical activity. Obesity rates are higher in rural areas than in urban and suburban areas. Increasing opportunities for exercise and access to healthy foods in neighborhoods, schools, and workplaces can help children and adults eat healthy meals and reach recommended daily physical activity levels. Examples of specific strategies to improve diet and increase exercise include:
Activity programs for older adults (SS) *
Offer group educational, social, or physical activities that promote social interactions, regular attendance, and community involvement among older adults
Farm to school programs (SE) *
Incorporate locally grown foods into school meals and snacks, often with visits from food producers, cooking classes, nutrition and waste reduction efforts, and school gardens
Farmers’ markets/stands (SE) *
Support multiple or single vendor markets where producers sell goods such as fresh fruit and vegetables, meat, dairy items, and prepared foods directly to consumers
Healthy food initiatives in food banks (SE)
Combine hunger relief efforts with nutrition information and healthy eating opportunities, often with on-site cooking demonstrations, recipe tastings, produce display stands, etc.
Places for physical activity (SS) *
Modify local environments to support physical activity, increase access to new or existing facilities for physical activity, or build new facilities
Prescriptions for physical activity (SS)
Provide prescriptions with individually tailored exercise plans, often accompanied by progress checks at office visits, counseling, activity logs, and exercise testing
School breakfast programs (SS)
Support programs that provide students with a nutritious breakfast in the cafeteria, from grab and go carts in hallways, or in classrooms
Screen time interventions for children (SS)
Encourage children to spend time away from TV and other screen media, often as part of a multi-faceted effort to increase physical activity and improve nutrition
* What Works for Health materials include rural-focused resources or studies
Choosing the Right Strategy for Your Community
To make sure you pick a strategy that fits your community best, be sure to consider the following questions:
- How similar is your target population (e.g., adolescents, seniors, or people with low incomes) to the population(s) the strategy has been shown to benefit?
- How similar are your goals to the outcomes the strategy has been shown to change?
- Can you implement the strategy just as it was studied? If not, how will you confirm your approach is effective too?
Involving a broad group of stakeholders, including local data and subject matter experts and members of the community, can help ensure your selected strategy is feasible and suitable for your community’s priorities and culture.
More strategies for rural areas
You can search What Works for Health (WWFH) for policies and programs that have been tested or implemented in settings like yours, or adapt strategies that have been tested elsewhere but seem like a good ‘fit’ for your community. Many of the strategies listed on the following pages have been tested or implemented in rural areas. New policies and programs are added regularly to WWFH, and existing entries are updated. This report reflects content as of June 24, 2016. Visit countyhealthrankings.org/whatworks to see the most current listings.
Strategies for Rural Areas
Strategies often affect health in multiple ways (e.g., school breakfast programs have been shown to increase academic achievement and healthy food consumption). Learn more about the specific outcomes and health factors each strategy has been shown to affect and the decision makers who can help move the strategy forward.
Credits
Recommended citation
University of Wisconsin Population Health Institute. What Works? Strategies to Improve Rural Health. July 2016.
Lead Authors
Alison Bergum, MPA
Bridget Catlin, PhD, MHSA
Julie Willems Van Dijk, PhD, RN
Karen Timberlake, JD
This publication would not have been possible without the following contributions:
Research Assistance
Marjory Givens, PhD, MSPH
Lael Grigg, MPA
Bomi Kim Hirsch, PhD
Amanda Jovaag, MS
Jessica Rubenstein, MPA, MPH
Jessica Solcz, MPH
Outreach Assistance
Matthew Call
Megan Garske
Communications and Website Development
Burness
Forum One
Robert Wood Johnson Foundation
Katrina Badger, MPH, MSW
Abbey Cofsky, MPH
Andrea Ducas, MPH
Michelle Larkin, JD, MS, RN
James Marks, MD, MPH
Joe Marx
Dwayne Proctor, PhD
Donald Schwarz, MD, MPH, MBA
Amy Slonim, PhD
Kathryn Wehr, MPH
Want printed copies of this report?
Get in touch with us today to request printed copies of this report to use in your communities
Want to share this report?
Select an icon below to share this report